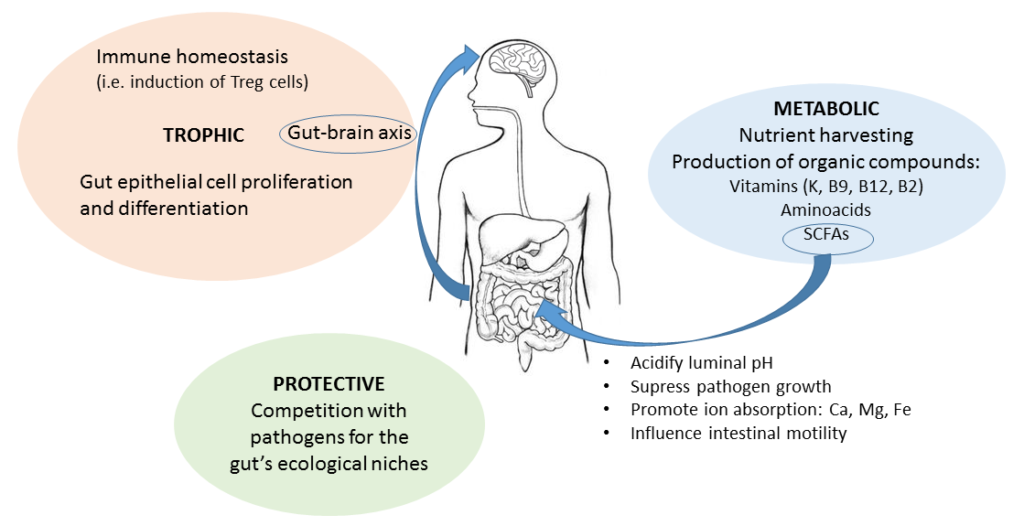
Functions of the gut microbiome can be classified in 3 categories:
- Metabolic
- Protective
- Trophic
Metabolic functions
The gut microbiota’s metabolism can be viewed as an extensión of the human metabolism. Others have decribed the gut microbiome as a ‘virtual organ’ because their joint metabolic activities are equivalent to those of a physical human organ.
Thank to this “extension” or “virtual organ” we can obtain nutrients and energy from food components that we are unable to digest. This is because they possess the enzymes necessary for these processes while humans, and mammals in general, have lost the genes encoding these enzymes.
Important examples of these functions are:
- Many microbes can extract energy from complex sugars in the diet that are indigestible for humans
- Colonic microbiota are able to ferment dietary carbohydrates and fibers that have arrived to the bowel undigested – some products of this fermentation are amino acids and short chain fatty acids (SCFAs), with beneficial effects in humans.
- The end products of some metabolic cycles of gut microbes happen to be key vitamins for human health
- They can also metabolise bile acids produced during digestión, which in turn influences cholesterol levels in humans
Protective functions
Our gut microbiota can also be viewed as a “shield” or “army” because they protect our gut from invasion by “bad microbes” with the potential to cause disease.
Their strategies and weapons are several:
- The “barrier strategy” – Simply by occupying their “homes”, the regions in the gut where they usually live (niches), they prevent other microbes from establishing themselves in the gut, where they shouldn’t be, and make havoc.
- The “starve the enemy” strategy – gut microbes feed on their nutrients on their homes, so there is none left for outsiders. The clever ones can even signal the human to stop producing an excess of a nutrient in order to prevént the outsiders from feeding on leftovers.
Both strategies are based on competition. Essentially, microbes compete for space and food. If the good microbes are where they are supposed to be, they are taking up space and food that can’t be used by bad microbes coming from outside or normal members of the microbiota that are harmless when they are occupying their niche, but harmful when they try to occupy a different one.
- The “mucus strategy” – This is another barrier strategy but this time the barrier is not formed by the microbes themselves but by the mucus layer that covers the gut lining. What can microbes do? They can give the order to increase the thickness of the mucus when the enemy approaches. Enemies are, for instance, inflammatory molecules or normal gut microbes that want to trespass the layer and go to other places in the body where they are harmful (formally called “translocation”)
- The bacteriocins weapon – Most gut microbes have their own weapons, called bacteriocins, that are small proteins (peptides) capable of killing or inactivating other microbes.
Trophic functions
- Communication with the gut lining cells – By interacting with these cells, the gut microbiota can influence their growth and also induce effects in other regions of the body. For example, such interactions can result in the cell switching off a particular gene and, when this gene is switched off, the effect is increased fat storage.
- The ‘microbiota-gut-brain axis’ – As strange as it may seem, this axis exists. It refers to the ability of gut microbes to affect our brain. Isn’t that incredible? Well, it is just Science unveiling the basis of the long well known gut-brain connection. They affect our brain biochemistry, our response to stress, our mood, behaviour and even our food cravings. More importantly, the gut microbiota colonization early in life affects the brain development.
- Education and regulation of the immune system – Again, a very important function in early life. Maturation of the gut microbiota and the immune system progress along the same time window in an infant’s life. This is from birth to about three years of life. During this key process, the microbiota and immune system talk to each other all the time. In essence, the microbiota are teaching the immune system what is friend and what is foe, and they promote the development of immune components by exposing themselves. Later in life, the microbiota-immune system communication continues and help balance pro-inflammatory and anti-inflammatory responses.